Andreas F Borkenstein,
1
Eva-Maria Borkenstein,
1
Sara Persson,
2
Gustav Muus,
3
Niels V Nielsen
3
1
Borkenstein & Borkenstein, Private Practice at Privatklinik der Kreuzschwestern Graz, Graz, 8010, Austria;
2
Skånes universitetssjukhus Malmö, Malmö, 214 28, Sweden;
3
Øjenhospitalet Danmark, Charlottenlund, 2920, DenmarkCorrespondence: Andreas F BorkensteinBorkenstein & Borkenstein Private Practice at Privatklinik der Kreuzschwestern Graz, Kreuzgasse 35, Graz, 8010, AustriaTel +43 316/331-38 80Fax +43 316 / 331-47 38 80Email
[email protected]
Abstract:
Age-related macular degeneration (AMD) is the leading cause of blindness in the developing world. AMD causes a substantial burden on patients, reducing independence, their ability to conduct daily activities, and increasing rates of cognitive decline and depression. There is a significant unmet need for patients with AMD, which will grow as the population ages and rates of disease increase. In the past, many studies have demonstrated a benefit when coexisting cataract formation is treated by removing the cloudy lens. AMD-lenses are intraocular implants designed to improve visual acuity in patients with AMD, avoiding the need for cumbersome manual vision aids and magnifiers. Many IOLs have been investigated in AMD, with differing mechanisms aimed at overcoming visual impairment. Most AMD studies use Early Treatment Diabetic Retinopathy Study (ETDRS) chart-based assessments of vision, but BCVA does not correlate with lesion size or pattern, especially in geographic atrophy, and may not be the most appropriate measure to effectively assess vision defects in AMD before or after a cataract surgery. One option is a simple functional assessment of vision related to activities of daily living (ADL), based on a reproducible, task-based questionnaire. The test consists of 6 assessments of ADL to be completed by patients before and after cataract surgery. Experiences highlight the importance of including an assessment of ADL in patients receiving an implant, which gives an effective measure of patient satisfaction. We would welcome the use of similar questionnaires in larger studies of patients, to validate its utility in a broader patient population. In this review article, we (Scandinavian-Austrian-cooperation) summarize lenses designed for implantation in patients with AMD, and how best to improve outcomes through proper patient selection, appropriate vision evaluation using quality-of-life related assessment, and pre- and post-operative care.
Keywords:
activities of daily life test, AMD, cataract, intraocular lens
Introduction
Age related macular degeneration is a progressive, debilitating disease. AMD is the leading cause of blindness in the developed world.
1
,
2
Currently there is no effective treatment for the majority of patients suffering from dry AMD.
3
Cataract and AMD often coexist in patients. In many cases, removing the cloudy lens can lead to a great benefit even in eyes with maculopathy.
4
Unfortunately, not all patients are offered this option, as some surgeons may not have sufficient experience with this special group of cataract patients. Similarly, a poor perception of the effects of cataract surgery in patients with AMD may have arisen due to widespread failure to afford sufficient attention to patient selection and patient expectations, and the perceived effectiveness of standard lenses.
An estimated 288 million people will have AMD globally by 2040.
1
80% of cases are non-neovascular atrophic/dry AMD.
5
Advanced dry AMD, or geographic atrophy (GA), results in irreversible vision loss.
6
Neovascular (wet) AMD is responsible for most severe central vision loss.
5
For patients with wet AMD, treatment with anti-VEGF has been shown to delay disease progression, but this requires a high burden of treatment.
7
,
8
To date, no treatment exists for dry AMD or geographic atrophy.
6
,
8
AMD causes a substantial burden on patients, reducing independence and their ability to conduct daily activities, and increasing rates of cognitive decline and depression.
2
Consequently, there is a significant unmet need for patients with AMD, which will grow as the population ages and rates of disease increase.
Assessments of Visual Acuity and Effects of Vision Loss
Most AMD studies use Early Treatment Diabetic Retinopathy Study (ETDRS) chart-based assessments of vision, such as Best Corrected (Distance) Visual Acuity (BCVA/BCDVA). But BCVA does not correlate with lesion size or pattern, especially in geographic atrophy,
6
and may not be the most appropriate measure to effectively assess vision defects in AMD.
Tests focused on function, such as vision and/or activities of daily living (ADL) are likely to be more relevant in patients with AMD. The NEI-VFQ-25 is a validated 25-question patient-reported outcome questionnaire that measures health indices, ADL and vision measures, and has been validated in AMD.
9
,
10
The Functional Reading Index (FRI) was developed as a novel patient-reported outcome (PRO) measure for clinical trials of geographic atrophy and tested in the Phase 2 and Phase 3 lampalizumab clinical trials.
11
Other measures include: maximum reading speed (which correlates with lesion size in geographic atrophy).
12
The Older American Resources and Services (OARS) ADL scale measures 14 activities (7 basic, 7 advanced);
13
having any AMD and advanced AMD increased the risk of experiencing total ADL impairment by 3- and 13-fold.
13
A computer-based assessment of finding objects, recognizing faces, and mobility-related stress, specific for patients with AMD, has also been formulated.
14
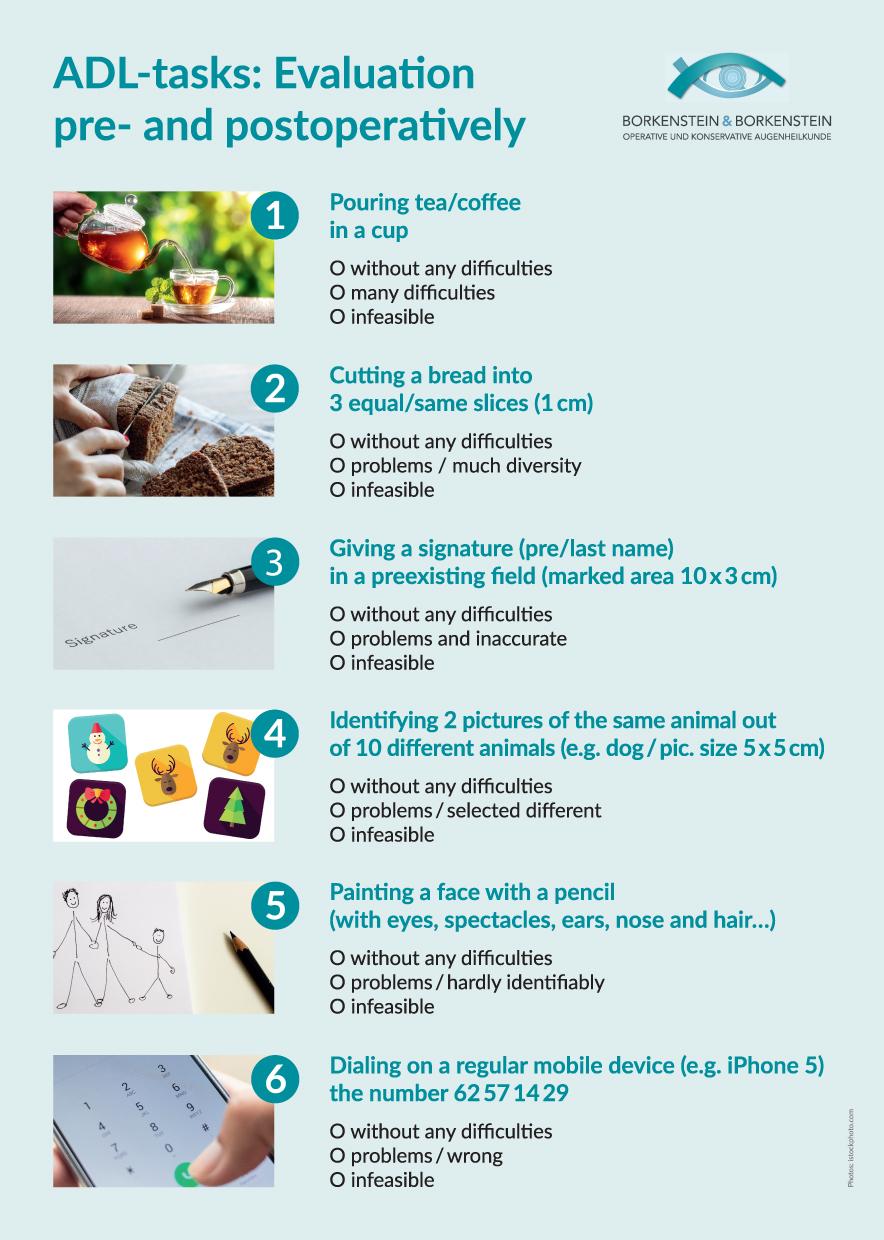
Nielsen, Borkenstein et al have developed a simple functional assessment of vision related to ADL, based on a reproducible, task-based questionnaire (
Figure 1
). The test consists of 6 assessments of ADL to be completed by patients before and after device implantation.
Figure 1
ADL and functional vision questionnaire. Evaluations take place prior to and after surgery with IOL implantation (Image courtesy Borkenstein & Borkenstein, Praxis für operative und konservative Augenheilkunde).
The tests require no specialist equipment and can be conducted at home or in clinic.
Unlike many other tests, these evaluations are objective – involving specific activities to be completed – rather than patient recollection or general impressions of improvement.
Borkenstein and Nielsen have trialed their assessment in a Danish-Austrian collaboration project with a case series of >100 patients. Overall, the weight of evidence indicates that ADL testing and better vision function assessments may more accurately reflect the benefits, or otherwise, of an AMD treatment – including IOL implants – when compared with static visual acuity measurements.
AMD-Lenses
AMD-lenses are intraocular implants designed to improve visual acuity in patients with AMD, avoiding the need for cumbersome manual vision aids and magnifiers.
4
,
15
Many devices have been investigated in AMD, with differing mechanisms aimed at overcoming visual impairment, these include the sub-category of intraocular telescopes, such as the Implantable Miniature Telescope (IMT), based on the Lipshitz Mirror Implant (LMI).
15
,
16
Available AMD-IOLs are summarized in
Table 1
and below - more comprehensive summaries of lens options have been published elsewhere:
4
,
15
Table 1
Summary of Available IOLs and Published Data
Intraocular lens for visually impaired people (IOL-VIP) (which requires pre- and post-operative training to promote the use of an alternative preferred retinal locus).
4
,
15
,
17
iolAMD, and its successor EyeMax Mono, which use a hyperaspheric design to improve the quality of retinal image to all areas of the macular within 10° of eccentricity of the foveal centre when compared with standard monofocal IOLs.
18–21
Scharioth Macula Lens, which aims to improve near vision of pseudophakic eyes, without affecting peripheral vision or binocularity at distances further than 15cm.
4
,
15
,
22–24
Fresnel Prism Intraocular Lens, which relocates the image to a healthy area of the retina.
4
,
25
Lentis Max IOL with a high magnification sector-shaped optical principle.
26
IOLs provide significant benefits for many patients, but are associated with intrinsic and patient-related limitations. Although the quality of data on effectiveness are variable, with limited prospective clinical trials, these devices typically improve single letter VA measures.
4
,
15
,
33
–
35
Quality of life improvements – based on functional measurements of vision – were reported for IMT using NEI-VFQ-25
27
and LMI and Lentis Max using non-validated measures.
16
Self-reported quality of life (using the NEI-VFQ-25) with IMT at 12 months resulted in a “clinically significant” improvement in composite score, vision-specific subscales and psychosocial vision-targeted subscales (albeit without accounting for the effects of cataract removal).
27
Patients completed a questionnaire pre- and post-implantation of LMI, assessing degree of difficulty on a 5-point scale for reading small print, large print, telling time and counting money, using a keyboard/dialing a telephone, watching television, and independent public mobility, resulting in a significant improvement in score from 11.16 (±1.72) to 4.5 (±0.83).
16
In the case studies of the Lentis Max, a quality-of-life assessment of autonomy (on a scale from 0 to 10) improved from 3 preoperatively to 6 postoperatively.
26
All mentioned implants appear to be generally well tolerated, although intraocular telescopes such as the IMT require more detailed pre-operative assessment for suitability, a period of training post-operatively and have higher rates of intra- and post-operative complications when compared with standard cataract surgery and monofocal intraocular lens implantation.
Typical adverse events include endothelial cell loss, transient increases in intraocular pressure, and glare.
15
Patient selection, expectation management, and rehabilitation is a necessity for many devices, including standard IOLs.
4
,
15
Improving Outcomes with AMD Lenses
Despite the potential benefits for patients from AMD lenses, many surgeons appear reluctant to recommend and implant them in their patients.
This may be due to concerns about surgical techniques, poor outcomes in previously treated patients or a misunderstanding of the best implants to select for their patients. In addition, there exists a deficit in the literature on evidence to support the standard of care – with most surgeons implanting standard monofocal IOLs of varying types on an unlicensed basis and published data failing to specify the precise nature of the IOLs implanted.
Confidence will be increased with surgeons having a clear understanding of which of their patients are suitable for device implantation, and which lens will best benefit which patients.
For example, the FDA approval of the IMT stated clear patient criteria necessary for implantation: patients must be ≥65 years of age, with VA between 20/160 and 20/800, have bilateral central scotomas associated with end-stage AMD, disciform scar or GA, and cataract. Preoperative tests must demonstrate an improvement of ≥5 letters with external visual aids.
28
,
29
Other lens manufacturers/healthcare professionals conducting studies should provide clear guidance of indications and contraindications for use of their lenses, in addition to use of the appropriate controls to deliver high-quality data on outcomes.
Key to a Successful Patient Outcome is Pre-Operative Management and Preparation
Patients must be suitable for implantation and likely to receive sufficient benefit from a device.
For example, implants that limit peripheral vision might not be suitable for individuals with mobility problems.
15
Expectation management is an essential component of patient preparation before device implantation. Vision will not be restored to pre-AMD a
cuity, and improvements may be modest (but sufficient to improve vision for ADL). In the UK, The National Institute for Health and Care Excellence (NICE) recommendations on the use of miniature lens systems/telescopes for AMD state:Ensure that patients understand the need to adapt to having a lens system implanted into 1 eye, the risk of early complications, and the uncertainties about long-term efficacy and safety.
30
Depression and poor mental health might make post-operative vision training difficult for some patients.
15
If expectations are not set appropriately, depression can become prevalent when treatment outcomes are lower than the patient expected.
8
Surgeons must be trained and suitably skilled to perform implantation.
For example, NICE states that these procedures should only be done by experienced cataract surgeons with appropriate training in the implantation of miniature lens systems”.
30
Patients must also understand the need for post-operative training with some lenses, and clinicians need to include suitable post-operative management into their care program.
Professional vision training should be offered to patients as necessary. Ongoing monitoring of safety and observation of results (training effect) is essential.
There are a number of practical considerations for achieving best outcomes with AMD lenses and the following questions should be addressed: Who is a suitable candidate? Who is not a suitable candidate? How should the appropriate device be selected?
As an illustration of how patient outcome may be assessed in daily life, beyond simple visual acuity measures, Borkenstein, Nielsen et al included in their Scandinavian-Austrian cooperation project a simple ADL quality of life questionnaire in their pre- and post-operative consultations.
Conclusion
There are multiple devices available for patients with AMD that are generally safe and provide visual improvements to help improve overall quality of life and enable greater independence for ADL.
Surgeons have the opportunity to create significant quality of life benefits by appropriately selecting and managing patients for the best clinical outcomes. A review of available publications and our own experience suggests that, with appropriate choice and care, patients are highly satisfied with the improvements in ADL conferred by AMD lenses.
There are currently no validated tests of functional vision or PROs specifically for patients with AMD; a kind of questionnaire is a simple, effective and objective assessment of vision-related ADL, suitable for use in the clinic as well as in trials, that could identify functional benefits from IOL implantation. The Macustar Consortium is aiming to identify and develop novel endpoints that detect functional vision loss or patient-relevant impact in intermediate AMD and will be accepted by regulators.
31
In addition to the mentioned questionnaire, other researchers are trying to identify suitable functional vision and ADL tests to be incorporated into a battery of AMD-appropriate options for clinicians.
11
,
14
Our own experiences from studies highlight the importance of including an assessment of ADL in patients receiving an IOL implant, which gives an effective measure of patient satisfaction. We would welcome the use of similar questionnaires in larger studies of patients, to validate its utility in a broader patient population. Moreover, we recommend building up a kind of international AMD-IOL task force to formulate decision-making aids and advice in a kind of White Paper.
Disclosure
The authors declare that they do not have any financial interest in products mentioned and report no conflicts of interest in this work.
References
1.
Wong L, Su X, Li X, Cheung C, Cheng CY, Wong T. Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: a systematic review and meta-analysis.
Lancet Glob Health
. 2014;2:e106–e116. doi:10.1016/S2214-109X(13)70145-1
2.
Prenner J, Halperin L, Rycroft C, Hogue S, Williams Liu Z, Seibert R. Disease burden in the treatment of age-related macular degeneration: findings from a time-and-motion study.
Am J Ophthalmol
. 2015;160:725–731. doi:10.1016/j.ajo.2015.06.023
3.
The Eye Diseases Prevalence Research Group. Prevalence of age-related macular degeneration in the United States.
Arch Ophthalmol
. 2004;122:564–572. doi:10.1001/archopht.122.4.564
4.
Grzybowski A, Wasinska-Borowiec W, ALio J, Amat-Peral P, Tabanero J. Intraocular lenses in age-related macular degeneration.
Graefes Arch Clin Exp Ophthalmol
. 2017;255:1687–1696. doi:10.1007/s00417-017-3740-8
5.
AAO PPP Retina/Vitreous Committee. Age-related macular degeneration PPP 2019; 2019. Available from:
https://www.aao.org/preferred-practice-pattern/age-related-macular-degeneration-ppp
.
Accessed
March
24
, 2020
.
6.
Fleckenstein M, Mitchell P, Bailey Freund K, et al. The progression of geographic atrophy secondary to age-related macular degeneration.
Ophthalmology
. 2018;125:369–390. doi:10.1016/j.ophtha.2017.08.038
7.
Gahn G, Khanani A. New therapies of neovascular AMD beyond anti-VEGF injections.
Vision
. 2018;2:15. doi:10.3390/vision2010015
8.
Mitchell P, Liew G, Gopinath B, Wong T. Age-related macular degeneration.
Lancet
. 2018;392:1147–1159. doi:10.1016/S0140-6736(18)31550-2
9.
Linblad A, Clemens T. Responsiveness of the National Eye Institute Visual Function Questionnaire to progression to advanced age-related macular degeneration, vision loss, and lens opacity: AREDS Report No. 14.
Arch Ophthalmol
. 2005;123:1207–1214.
10.
Sivaprasad S, Tschosik E, Kapre A, et al. Reliability and construct validity of the NEI VFQ-25 in a subset of patients with geographic atrophy from the phase 2 Mahalo study.
Am J Ophthalmol
. 2018;190:1–8. doi:10.1016/j.ajo.2018.03.006
11.
Kimel M, Leidy N, Tschosik E, et al. Functional Reading Independence (FRI) index: a new patient-reported outcome measure for patients with geographic atrophy.
IOVS
. 2017;57:6298–6304.
12.
Varma R, Souied E, Tufail A, et al. Maximum reading speed in patients with geographic atrophy secondary to age-related macular degeneration.
IOVS
. 2018;59:AMD195–AMD201.
13.
Gopinath B, Liew G, Burlutsky G, Mitchell P. Age-related macular degeneration and 5-year incidence of impaired activities of daily living.
Maturitas
. 2014;77:263–266. doi:10.1016/j.maturitas.2013.12.001
14.
Higgins B, Taylor D, Crabb D. Assessing everyday visual function in dry AMD - what matters to the person?
Eye News
. 2019;25. Available from:
https://www.eyenews.uk.com/features/ophthalmology/post/assessing-everyday-visual-function-in-dry-amd-what-matters-to-the-person
.
15.
Dunbar H, Dhawahir-Scala F. A discussion of commercially available itra-ocular telescopic implants for patients with age-related macular degeneration.
Ophthalmol Ther
. 2018;7:33–48. doi:10.1007/s40123-018-0129-7
16.
Agarwal A, Lipshitz I, Jacob S, et al. Mirror telescopic intraocular lens for age-related macular degeneration - Design and preliminary clinical results of the Lipshitz macular implant.
J Cataract Refract Surg
. 2008;34:87–94. doi:10.1016/j.jcrs.2007.08.031
17.
Orzalesi N, Pierrottet C, Zenoni S, Savaresi C. The IOL-Vip System: a double intraocular lens implant for visual rehabilitation of patients with macular disease.
Ophthalmol
. 2007;114:860–865. doi:10.1016/j.ophtha.2007.01.005
18.
Qureshi M, Robbie S, Hengerer F, Auffarth G, Conrad-Hengerer I, Artal P. Consecutive case series of 244 age-related macular degeneration patients undergoing implantation with an extended macular vision IOL.
Eur J Ophthalmol
. 2018;28:198–203. doi:10.5301/ejo.5001052
19.
Hengerer F, Auffarth G, Robbie S, Yildirim T, Conrad-Hengerer I. First results of a new hyperaspheric add-on intraocular lens approach implanted in pseudophakic patients with age-related macular degeneration.
Ophthalmol Retina
. 2018;2:900–905. doi:10.1016/j.oret.2018.02.003
20.
Robbie S, Tabanero J, Artal P, Qureshi M. Initial clinical results with a novel monofocal-type intraocular lens for extended macular vision in patients with macular degeneration.
J Refract Surg
. 2018;34:718–725. doi:10.3928/1081597X-20180831-01
21.
Borkenstein A, Borkenstein EM. A case report detailing use of a new intraocular lens with advanced technology, designed specifically for patients with center-involving macular disorders.
Medicine
. 2019;98:e16583. doi:10.1097/MD.0000000000016583
22.
Nekolova J, Rozsival P, Sin M, Jiraskova N. Scharioth Macula Lens: a new intraocular implant for low-vision patients with stabilized maculopathy - first experience.
Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub
. 2017;161:206–209. doi:10.5507/bp.2017.014
23.
Bereczki Á. Experiences with the Scharioth Macula Lens - new hope for patients with dry macula degeneration.
Rom J Ophthalmol
. 2019;63:128–134. doi:10.22336/rjo.2019.19
24.
Srinivasan S, Scharioth G, Riehl A, et al. Implantation of Scharioth macula lens in patients with age-related macular degenration: results of a propsective European multicentre clinical trial.
BMJ Open Ophthalmol
. 2019;4:e000322. doi:10.1136/bmjophth-2019-000322
25.
Potgeiter F, Claoue C. Safety and efficacy of an intraocular Fresnel prism intraocular lens in patients with advanced macular disease: initial clinical experience.
J Cataract Refract Surg
. 2014;40:1085–1091. doi:10.1016/j.jcrs.2013.10.049
26.
Borkenstein A, Borkenstein EM. Cataract surgery with implantation of a high-add intraocular lens LENTIS
®
MAX LS-313 MF80 in end-stage, age-related macular degeneration: a case report of magnifying surgery.
Clin Case Rep
. 2018;7:74–78. doi:10.1002/ccr3.1912
27.
Boyer D, Bailey Freund K, Regillo C, Levy M, Garg S. Long-term (60-month) results for the implantable miniature telescope: efficacy and safety outcomes stratified by age in patients with end-stage age-related macular degeneration.
Clin Ophthalmol
. 2015;9:1099–1107. doi:10.2147/OPTH.S86208
28.
Hau V, London N, Dalton M. The treatment paradigm for the implantable miniature telescope.
Ophthalmol Ther
. 2016;5:21–30. doi:10.1007/s40123-016-0047-5
29.
US Food & Drug Administration; July 07, 2010. Available from:
https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfpma/pma.cfm?id=P050034
.
Accessed
April
01
, 2020
.
30.
National Institute for Health and Care Excellence; September 28, 2016. Available from:
https://www.nice.org.uk/guidance/ipg565/resources/miniature-lens-system-implantation-for-advanced-agerelated-macular-degeneration-pdf-1899872049404869https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfpma/pma.cfm?id=P050034
.
Accessed
March
25
, 2020
.
31.
Finger R, Schmitz-Valckenberg S, Schmid M, et al. MACUSTAR: development and clinical validation of functional, structural, and patient-reported endpoints in intermediate age-related macular degeneration.
Opthalmol
. 2019;241:61–72. doi:10.1159/000491402
32.
ALio J, Mulet E, Ruiz-Moreno J, Jose Sanchez M, Galal A. Intraocular telescopic lens evaluation in patients with age-related macular degeneration.
J Cataract Refract Surg
. 2004;30:1177–1189. doi:10.1016/j.jcrs.2003.10.038
33.
Hengerer F, Artal P, Kohnen T, Conrad-Hengerer I. Initial clinical results of a new telescopic IOL implanted in patients with dry age-related macular degeneration.
J Refract Surg
. 2015;31:158–162. doi:10.3928/1081597X-20150220-03
34.
Tabanero J, Qureshi M, Robbie S, Artal P. An aspheric intraocular telescope for age-related macular degeneration patients.
Biomed Optics
. 2015;6:1010–1020. doi:10.1364/BOE.6.001010
35.
Qureshi M, Robbie S, Tabanero J. Injectable intraocular telescope: pilot study.
J Cataract Refract Surg
. 2015;41:2125–2135. doi:10.1016/j.jcrs.2015.03.021